Throughout the COVID-19 pandemic, I have been washing my hands with vigilance to prevent the spread of germs. As a result, the skin on my hands have become calloused on some parts and mostly dry, with cuts and slight bleeding on occasion. I thought this was inconvenient, but when I learned about children with a rare genetic skin disease, I stopped feeling sorry for myself and dug a bit deeper into their plight. After all, my skin issues are just due to excessive hand washing (which everyone should be doing anyway!); these poor kids have to live with this painful disease, known as dystrophic epidermolysis bullosa, for their entire lives.

Dystrophic Epidermolysis Bullosa
The term “dystrophic epidermolysis bullosa” (DEB) is used to describe a specific type of skin disorder where the skin is extremely fragile, causing it to blister and wound easily. The skin can peel away or blister due to minor injury or friction from bending one’s elbow or through normal digestion, and sometimes even if the person is barely touched. (The images of patients with this disorder are very graphic and heartbreaking, which is why we haven’t shared any this time.)
Because the skin is the most extensive organ on the body and includes epithelial layers in the mouth and digestive system, this disorder affects not just the outer skin, but also the lining of the eyes and organs like the esophagus. I can’t even imagine how the affected skin would react to intense sunlight, but people who suffer from the recessive form of DEB have a high risk of developing squamous cell carcinoma, likely because of the unusually constant need to replenish skin that keeps being sloughed off at an elevated rate. The most severe form of DEB is known as “severe generalized recessive DEB,” in which the skin ailments described above can cause loss of vision, disfigurement, and malnutrition due to the difficulty in eating food. The disorder is known to be caused by mutations in a collagen gene called COL7A1. Unfortunately, to date, there is no cure for this severe form of DEB.
The Importance of Collagen in Normal Skin Health
As skin is the largest organ, and we already know from DEB patients that skin needs reinforcement from collagen to maintain its normal structure and function, it is no surprise that collagen comprises the most abundant protein in the body. Collagen acts as a critical structural protein to strengthen the architectural elements of the body, including skin, internal organs, bone, teeth, and muscles.
Normally, collagen winds together as three chains forming a triple helix, somewhat like a suspension cable for a bridge. The collagen chain is highly enriched in the flexible amino acid glycine, as well as proline and a modified proline called hydroxyproline. It is thought that this amino acid composition lends itself to the tight, reinforced structure of collagen. (Figure 1)
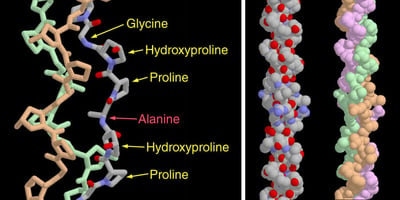
Figure 1: The unique structure of a collagen triple helix. Source: Protein Data Bank
Collagen is a common ingredient in protein-based supplements and is also a cosmetic filler for people who want fewer wrinkles or fuller lips. Because of its function in strengthening skin, collagen would serve as a logical potential therapy for DEB and other skin diseases.
Treating Skin Disorders Through Collagen Gene Therapy
Since severe recessive DEB is caused by the loss of function in the COL7A1 gene, one treatment strategy is to reintroduce the gene product to the skin of the affected person, if not the entire genome. Various studies and therapeutic trials, including this study from Stanford University, are dedicated toward a practical treatment option that could reinsert, even temporarily, the COL7A1 gene into the outer skin cells to at least alleviate the scarring and painful symptoms.
The group at Stanford led by dermatologist Peter Marinkovich recently reported on their therapeutic trial involving a topical ointment that delivered a gene encoding COL7A1. 1 The use of a herpes simplex virus vector to accommodate the large gene sounds scary, and would have made me think that it would cause a severe inflammatory response to the viral delivery system. However, the researchers took advantage of the natural immune evasive abilities of herpes virus and reported no adverse effects from applying the treatment. 1
Patients receiving the topical gel treatment fared very well, showing significant healing of skin compared to the placebo group. The fact that it is essentially a skin cream makes this type of treatment easy and convenient relative to other strategies. The success of this type of therapy has encouraged further studies into applying the strategy towards other skin and mucosal surfaces, as well as for cosmetic purposes. 1
More Skin In the Game: Limitations of a Topical Treatment and Exploring Future Directions
Marinkovich and colleagues did caution that there would be limits to this type of treatment, however encouraging the initial results would appear. For example, the topical gel was only expected to work on open wounds on recessive DEB patients, as intact skin is resistant to infection by the herpes virus vector used to deliver the COL7A1 gene. 1 Another unfortunate obstacle is that even the healed skin will eventually turn over, and since the gene therapy appears to be transient, the gel would need to be reapplied frequently. There are challenges involved with using a CRISPR-based approach to gene therapy, but that would seem to be a future direction that would make the treatments more permanent without having to resort to skin grafts or engineered stem cell therapies.
The study suggested that a future goal would be to treat the eyes, inner mouth, esophagus, and other epithelial and mucosal surfaces that suffer from constant stress and friction. While this was not explicitly discussed, I do wonder how bad the gel would taste going down the gullet, and whether the vector would survive the stomach acids and digestive enzymes on its way toward the intestines and colon. And if the topical gel cannot penetrate non-wounded tissue, it may not be very effective for those internal areas even if it can survive the digestive system or immune surveillance.
Despite the challenges and apparent shortfalls, a topical gene therapy is a very exciting approach that can potentially be applied to other diseases. Alleviating such a painful ailment, even temporarily, as easily as me putting lotion on my hands is surely a relief for these patients, who no longer have to fly all over the country to special hospitals and can instead treat themselves in the comfort of their homes. Providing a means to improve the patient’s quality of life at a reasonable expense with ease of application is a health professional’s dream, and this is an encouraging first step.
An Exciting Update
Just one year after we first described this life-changing therapy, the FDA has approved the topical treatment for DEB patients! The gene therapy is carried by a non-replicating herpes simplex 1 virus and helps restore COL7A1 expression to help heal the skin wounds. The drug is known as Beremagene geperpavec, branded as Vyjuvek, and was approved in May of 2023. It is difficult to predict the speed of progress sometimes, but a year's time is an indicator of how important and effective this therapy is to improve the quality of life for patients suffering this rare disease. Of course, the ointment only alleviates symptoms and doesn't actually cure the genetic abnormality, so further research and clinical trials will have to be conducted to find a more permanent therapy. Applying a cream once a week is easy and convenient, however, and represents a much better approach than what was done previously.
You can learn more by reading this news brief from Nature and also check out this snapshot from Cell.
Reference
- Gurevich et al. (2022) “In vivo topical gene therapy for recessive dystrophic epidermolysis bullosa: a phase 1 and 2 trial.” Nature Medicine 28:780-788.
Please feel free to peruse ABclonal’s Collagen Type VII related products.