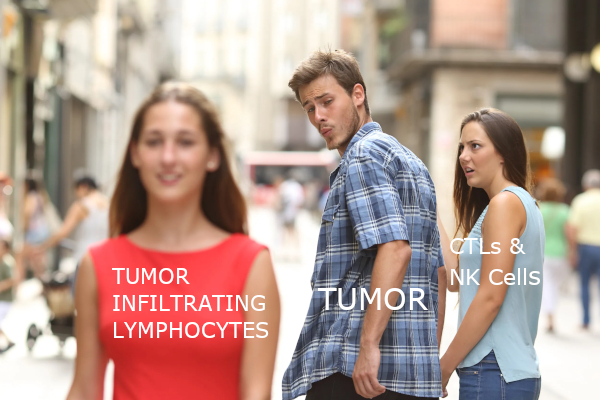
With a background in both immunology and cancer biology, I’ve always had a fascination with the interplay between the body’s immune system and any tumors that might pop up. Originally, it made sense that the immune system would actively seek out and destroy cancerous cells, but the emerging consensus is that the interactions between cancers and host immunity is far more complex. In addition to growing new blood vessels and reprogramming metabolic processes, there appears to be some imbalance between avoiding immune cells while also promoting tumor-infiltrating inflammatory cells to promote its growth. 1 (Figure 1) Trying to dissect this apparent contradictory relationship between tumors and host immunity remains a hot topic.
A healthy immune system requires a series of checkpoints to ensure self tolerance and prevent damage to other tissues during immune response. Binding of costimulatory signal transduction molecules (such as CD28, ICOS, GITR) on T cells to their receptors (such as CD80/CD86, ICOSL, GITRL) on antigen presenting cells (APCs) may contribute to T cell activation. However, in some states, inhibitory signals of T cell activation and response occur during the involvement of T cell receptors. These signals are generated by proteins involved in immune checkpoints (eg, PD-1, CTLA-4, TIM-3, and LAG3). Usually PD-1 and CTLA-4 immunological checkpoint proteins are upregulated in T cells infiltrating tumors and bind to their respective ligands, PD-L1 (ligand B7-H1)/PD-L2 (ligand B7- DC) and CD80/86, and down-regulate T cell responses. Immunological checkpoint ligands are often upregulated in cancer cells as a means of evading immune detection. Therefore, immunotherapy by blocking immunological checkpoint protein activation of anti-tumor immunity has become a popular research subject for cancer therapy.